Aggression
OXIDATIVE STRESS, AMYLOID & ULTRASOUND
Aggression (as well as agitation, delusions, paranoia, psychosis, mania, bipolar affective disorder, etc.) after C-19 injection in the VAERS database
VAERS ID:1786808
Age:12.0
Sex:Male
Write-up:
A 12-year and 9-month-old male patient received the second dose of bnt162b2 (COMIRNATY), via an unspecified route of administration on 25Sep2021 (at the age of 12-year-old) as DOSE 2, SINGLE for COVID-19 immunisation.
On 28Sep, a contact was received from police reporting that the patient attempted to jump from the 5th floor and swung a knife, during which he was protected.
VAERS ID:1592992
Age:20.0
Sex:Male
Write-up:
Around 10 hours after the injection of the shot I began to feel fever and soon after began to hallucinate, hear voices and violently shake.
I began to hurt myself by hitting and pulling my hair out. I then ran out into the street in my underwear and called 911 as I was very confused and concerned I would seriously harm myself and others. I was handcuffed by the police but ran away.
After being secured and transported to hospital I was administered a sedative drug and released after I was no longer involuntarily shaking.
VAERS ID:2400581
Age:56.0
Sex:Female
02/10/2021around 8:00 am i could hear my nephew doing his online schooling, For some unknown reason this angered me, this was very unusual behavior for me I stumbled to the kitchen and started a confrontation with him and i ended up striking him at some point,
the school had no choice but to call police and report my abuse . The police came to our home at appoximatly 2:00 pm They question nephew, my husband, my mother, and myself only to discover this was very unusual behavior from me and i had never done anything like that before. My husband explained that I had been ill since I Recieved the covid vaccine, the vomiting, dizziness, inability to walk on my own irrational behavior, forgetfulness and the sleepiness.
VAERS ID:1138921
Age:76.0
Sex:Male
Write-up:
About 4 hours after the vaccination the patient got agitated and did not know who I was and went next door and told the neighbor to call the police to get me out of his house. His memory of me came back about 4 hours later. 4 days later it happened again only more agitated. His memory came back again, but not for several hours.
The 3rd episode happened 4 days after that and the agitation escalated into total psychosis and he tried to stab me with a steak knife.
The police took him to the hospital and the doctors have been trying to adjust he meds to keep him from getting violent. He has been in a month now. Prior to the vaccination on February 20th things were normal, went out to lunch, he knew who I was.
VAERS ID:1631891
Age:35.0
Sex:Male
Write-up:
Violence and verbal abuse; Memory impairment;
On 10-Aug-2021, the patient woke up as usual. The patient used abusive language and violence against the father and child. The patient looked different from usual. The patient was unable to have a conversation. The patient was unable to recognize his family members and boss.
Sender''s Comments: Based on the current available information and temporal association between the use of the product and the onset of the events, a causal relationship cannot be excluded.
VAERS ID:1723879
Age:34.0
Sex:Female
Write-up:
A couple days after shot, symptoms of psychosis began. Talking to someone that I thought was there but wasn''t actually there, Full on conversations, was unable to sleep that night due to this. Hallucinations of people being there when they were not. Memory Loss, dysnomia, inability to recall events as they truly happened. Believing conversations were real when they never truly happened.
Extreme agitation, irritability, violence, inability to focus, extreme impulsivity and almost manic behavior, racing thoughts, increased blood pressure.
It is now 3 months since I have had the first dose, I do not feel my normal self and I believe the vaccination triggered the psychosis.
VAERS ID:1315459
Age:25.0
Sex:Male
Write-up:
On the morning of 27Apr2021 (4 days after the vaccination), the patient experienced mental state abnormal and committed suicide. The patient who worked as a clinical laboratory technician for the hospital was running riot as discovered taking out potassium chloride (KCL) without permission on 27Apr2021. He was finally hold down. He was diagnosed by psychiatric consultation with Paranoid state/Mental disorder. The patient was being transported to a psychiatric hospital in a passenger car by his family. But on the way, the patient jumped out of the car overcoming the family''s restraint and died.
VAERS ID:2431026
Age:26.0
Sex:Male
Write-up:
27-year-old male with history of hypertension and mood disorder was brought to the hospital by the cops since he was noted to have paranoid thoughts, hallucinations, homicidal ideations and aggressive behavior.
The police found him yelling on the streets and fighting. Per notes, patient told that someone stole his father''s car business and he wanted to kill him. He also endorsed suicidal thoughts per notes.
He mentions to have received 2 doses of the vaccine in 2021. When I examined the patient, he did not want to go into details of why he was having homicidal and suicidal ideations.
…
Aggression and oxidative stress in scientific articles
https://journals.sagepub.com/doi/10.1177/08902070241233027 Self-reported aggression is related to oxidative stress in men and women
February 21, 2024
Abstract
Aggression is an important element of social behavior. Increased aggression has been observed in many mental disorders, posing a serious public health concern. However, the proximal biological mechanisms underlying an individual’s proneness to aggressive behavior remain poorly understood.
Studies in both non-human animals and humans with aggressive disorders have shown that aggression is positively related to oxidative stress levels.
We found that 8-OH-dG level was positively related to physical aggression. Our findings provide preliminary evidence that healthy individuals with higher levels of oxidative stress are more physically aggressive.
We hypothesize that evaluating markers of oxidative stress levels may be useful for screening healthy populations to identify individuals who may be particularly susceptible to the development of mental issues related to aggression.
https://mdpi-res.com/d_attachment/ijms/ijms-24-00915/article_deploy/ijms-24-00915-v2.pdf?version=1673518809 Understanding the Role of Oxidative Stress, Neuroinflammation and Abnormal Myelination in Excessive Aggression Associated with Depression: Recent Input from Mechanistic Studies
Published: 4 January 2023
Abstract: Aggression and deficient cognitive control problems are widespread in psychiatric disorders, including major depressive disorder (MDD). These abnormalities are known to contribute significantly to the accompanying functional impairment and the global burden of disease. Progress in the development of targeted treatments of excessive aggression and accompanying symptoms has been limited, and there exists a major unmet need to develop more efficacious treatments for depressed patients. Due to the complex nature and the clinical heterogeneity of MDD and the lack of precise knowledge regarding its pathophysiology, effective management is challenging. Nonetheless, the aetiology and pathophysiology of MDD has been the subject of extensive research and there is a vast body of the latest literature that points to new mechanisms for this disorder.
Here, we overview the key mechanisms, which include neuroinflammation, oxidative stress, insulin receptor signalling and abnormal myelination.
We discuss the hypotheses that have been proposed to unify these processes, as many of these pathways are integrated for the neurobiology of MDD.
We also describe the current translational approaches in modelling depression, including the recent advances in stress models of MDD, and emerging novel therapies, including novel approaches to management of excessive aggression, such as anti-diabetic drugs, antioxidant treatment and herbal compositions.
Based on the literature reviewed here, increased aggression is also associated with oxidative stress and neuroinflammation, which can be a potential target of pharmacotherapy for MDD patients suffering from uncontrollable aggressive behaviour. As such, the potential of antioxidant treatment in the management of aggression has been proposed in several studies [62,63,66,67,238]. Decreased levels of endogenous antioxidants, such as glutathione and superoxide dismutase, lead to an increase in oxidative stress, which in turn produces anxiogenic behaviour and aggression in mice [256]. Oxidative stress decreases expression of the MAOA gene, whose low activity has been implicated in violence and aggression [257]. The reactive oxygen species level was elevated in the brains of mice subjected to repeated forced swimming., but this increase was reversed using clomipramine, a tricyclic antidepressant [258]. Antioxidant and anti-inflammatory treatments are anticipated to be free from typical side effects of traditional anti-anxiety drugs and SSRIs [259]. Taking into account the above-reviewed data, it can be hypothesized that the use of compounds with anti-inflammatory and antioxidant properties may be a beneficial strategy for the depressive-like symptoms associated with excessive aggression and the accompanying molecular alterations.
9. Conclusions
During the last decade, the classic monoamine theory of depression and associated symptoms of MDD has been adjusted and extended considerably. An increasing body of evidence points to brain alterations occurring not only in classic neurotransmitters but also in neuronal connectivity that could be caused by disrupted myelination and triggered by an increase in oxidative stress and neuroinflammation. These alterations were observed both in clinical and animal studies of depressive disorder accompanied by pathological aggression. A recently hypothesized “triad” of inter-related molecular mechanisms of neuroinflammation, myelination and IR signaling might underlie the deficiency in brain connectivity contributing to the pathophysiology of MDD and impulsivity control in depressed patients (Figure 1). Consequently, this view suggests that compounds targeting oxidative stress, neuroinflammation and the activity of oligodendroglia may be considered as new approaches to offer more specific and effective treatment of the depressive symptoms associated with excessive aggression.
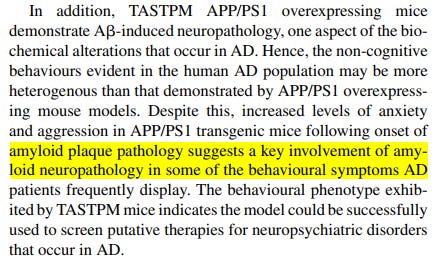
Aggression and amyloid plaque formation in scientific articles
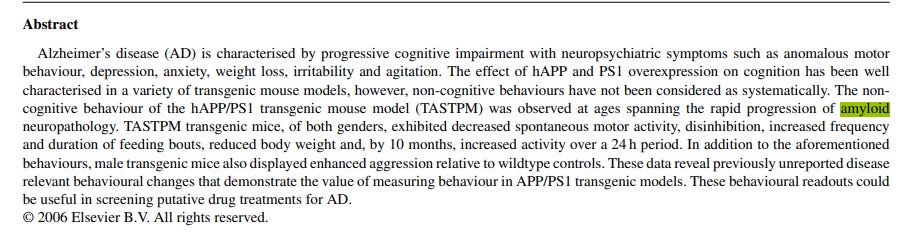
http://www.metris.nl/media/documents/laboras/Publications/2007%20-%20Pugha%20-%20Behaviors%20in%20APP_PS1%20Transgenic%20model%20for%20Alzheimer.pdf Non-cognitive behaviours in an APP/PS1 transgenic model of Alzheimer’s disease
Available online 16 January 2007
https://alz-journals.onlinelibrary.wiley.com/doi/pdf/10.1016/j.jalz.2016.06.366 EFFECTS OF CORTICAL AMYLOID B DEPOSITION ON THE INCIDENCE AND PREVALENCE OF NEUROPSYCHIATRIC BEHAVIORS IN THE ELDERLY
O1-13-04
Conclusions:
Amyloid+ MCI have higher prevalence and incidence over time of neuropsychiatric behaviors. In MCI, amyloid pathology is a significant risk factor for developing apathy, anxiety, and agitation.
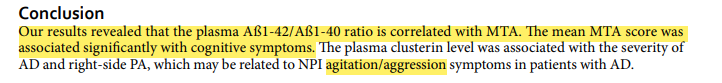
http://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC5506051&blobtype=pdf Plasma biomarkers are associated with agitation and regional brain atrophy in Alzheimer’s disease
Published online: 11 July 2017
One of the most intriguing things to me in psychiatry is the push-pull between specific diagnoses and common factors. Are all psychiatric disorders basically the same or are they radically different from one another?
For instance:
Is schizophrenia different from bipolar disorder? And if so, how?
Is major depression different from panic disorder? And if so, how?
Do you have two, three, or four different problems? Couldn’t your several diagnoses all result from a single problem in your brain, a set of circuits or brain centers with abnormally increased or decreased activity that cause either a few or a lot of symptoms?
Overall, the research on brain circuits generally gives support to lumpers: It’s generally the same circuits that go awry in nearly all psychiatric disorders, though perhaps with different emphasis for different disorders.
Which gets me to N-acetylcysteine.
[ALSO PLEASE NOTE: the use of NAC for psychiatric symptoms is an off label use. The only FDA approved indication for NAC is in treatment to prevent serious liver damage from acetaminophen poisoning. As such, if you are planning to use NAC for psychiatric or other medical symptoms please discuss with your physician to make sure it is safe and potentially beneficial]
Why does NAC help many people with psychiatric diagnoses? Why does it work across so many conditions? This is the intriguing thing, in my eyes. Are its benefits a result of its anti-inflammatory effects? Or some other mechanism? On a clinical level, in day-to-day work with patients, NAC seems to help with ruminations, with difficult-to-control extreme negative self-thoughts. Such thoughts are common in depression and anxiety disorders, and also in eating disorders, schizophrenia, OCD, etc. I’ve seen it help patients with such disorders when many other things, medicines or psychotherapies, have not helped much.
NAC doesn’t always work, but when it does, troubling irrational thoughts gradually decrease in intensity and frequency and often fade away.
…
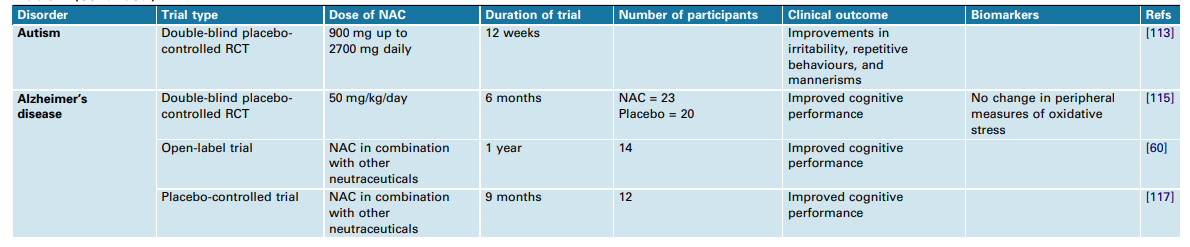
http://ponderapharma.com/wp-content/uploads/2014/06/The-promise-of-N-acetylcysteine-in-neuropsychiatry.pdf The promise of N-acetylcysteine in neuropsychiatry
N-Acetylcysteine (NAC) targets a diverse array of factors germane to the pathophysiology of multiple neuropsychiatric disorders including glutamatergic transmission, the antioxidant glutathione, neurotrophins, apoptosis, mitochondrial function, and inflammatory pathways.
This review summarises the areas where
the mechanisms of action of NAC overlap with known pathophysiological elements, and offers a pre´ cis of current literature regarding the use of NAC in disorders including cocaine, cannabis, and smoking addictions, Alzheimer’s and Parkinson’s diseases, autism, compulsive and grooming disorders, schizophrenia, depression, and bipolar disorder.
There are positive trials of NAC in all these disorders, and although many of these require replication and are methodologically preliminary, this makes it one of the most promising drug candidates in neuropsychiatric disorders. The efficacy pattern of NAC interestingly shows little respect for the current diagnostic systems. Its benign tolerability profile, its action on multiple operative pathways, and the emergence of positive trial data make it an important target to investigate.
Role in oxidative homeostasis The brain is acutely sensitive to changes in redox status. The high metabolic activity of this organ is a persistent source of oxidative species, as utilization of O2 by energy-generating mitochondria constantly generates oxygen free radicals [24,25]. Neurotransmitter activity also generates free radicals, with autooxidation of dopamine and excitotoxicity related to glutamatergic signaling being important sources of oxidative stress [10,20]. Neurons rely on the integrity of extensive axonal membranes for efficient information signaling, and these membranes, high in polyunsaturated fatty acids, are vulnerable to free radical damage. Compounding these factors, the levels of endogenous antioxidants in the brain are low relative to other highly metabolically active organs. At the far end of the spectrum, excessive oxidative stress can lead to neurotoxicity and cell death, but redox systems also play an important regulatory role in the modulation of enzyme activity intracellular signalling systems, and receptors (beyond the scope of this review, but discussed in [26]). One example of this is the redox regulation of the NMDA receptor, as discussed above. Thus, even moderate perturbations of the redox balance can alter neuronal function, even in the absence of overt toxicity and neuronal damage.
Use in psychiatry
There is a growing body of literature of potential benefit of NAC in a wide range of neuropsychiatric disorders.
Concluding remarks
Given the paucity of new drug development, NAC is a promising novel therapeutic option for a diverse range of neuropsychiatric disorders.
To date, two divergent hypothetical paths have converged on NAC as a potential treatment. Firstly, oxidative stress and GSH deficiency has driven the focus on NAC in schizophrenia, bipolar disorder, and depression. Superadded to this, and in parallel, addiction research has hypothesised NAC to be active via the modulation of glutamate and the cystine–glutamate antiporter [76]. However, knowing that NAC also has effects on inflammatory pathways, neurotrophins, mitochondrial function, and oxidative stress, its true efficacy profile may turn out to be due to preferential effects on any of these, or a summative interaction of influences on a variety of pathways. Unravelling these complexities has the potential to open up new avenues for the development of novel psychotropic agents.
Since the formation of amyloid-producing proteins is already implicated in HCCAA and other diseases, researchers have studied whether drugs that reduce the aggregation of these proteins have the potential to reduce the toxic oligomers, or polymers made up of a few different molecules.
“While this is a rare disease, most patients diagnosed with HCCAA die within five years of their first stroke, so there is an incredible need to study this genetic disorder and find effective treatment options,” said Hakon Hakonarson, MD, PhD, Director of the Center for Applied Genomics at CHOP and lead author of the study.
Since the formation of amyloid-producing proteins is already implicated in HCCAA and other diseases, researchers have studied whether drugs that reduce the aggregation of these proteins have the potential to reduce the toxic oligomers, or polymers made up of a few different molecules. To properly study this strategy in HCCAA, the research team created cell lines expressing both wild type and L68Q-mutant hCC and then attempted to non-toxically interfere with the aggregation of the amyloid-producing proteins. The researchers also studied a supplement called N-acetyl-cysteine (NAC), which is sometimes prescribed to break up mucous in the lung and has also been shown to protect against the toxic liver damage caused by an acetaminophen overdose, to determine whether it had an effect on hCC-amyloid protein deposits in skin biopsies of patients with a known diagnosis of HCCAA.
The researchers found that treating these cell lines with NAC breaks the oligomers into monomers, or molecules that have been separated from the chain that brings them together. This in turn helps to prevent the formation of amyloid-producing proteins that lead to the amyloid deposits implicated in strokes and other impairments. The researchers also performed skin biopsies on six patients with the L68Q-hCC variant taking NAC to determine levels of hCC-amyloid protein deposits following treatment. Five of the six patients saw between a 50% and 90% reduction of L68Q-hCC levels, suggesting that this variant is a clinical target for reducing agents such as NAC. This proof-of-concept study led to a clinical trial to see if these results are observed in a larger patient cohort.
“Amyloids cannot precipitate without aggregating, so if we can prevent that aggregation with a drug that is already available, then we could make an incredible difference in the lives of these patients,”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7988011/pdf/41467_2021_Article_22120.pdf
In addition to oxidative stress and amyloid plaque formation, there is another interesting link between aggression and... ULTRASOUND.
In another study, male Balb/c mice were subjected to a 3-week ultrasound radiation in 20-45 kHz frequencies ranges, which was recently shown to evoke emotionally negative state and affective disturbances.
It was found that this challenge has induced aggressive-like changes.
ALLEGED MIND CONTROL IN RWANDA AND MIND CONTROL IN BAGHDAD? THEY WERE TECHNICALLY FEASIBLE....
https://en.wikipedia.org/wiki/Sonic_weapon
https://jbino.com/docs/Issue04_01_2020.pdf NAPHAZOLINE NITRATE, BISACODYL AND GUTTALAX TREAT MICROWAVE SONIC EFFECTS
Sonic and ultrasonic weapons (USW) are weapons of various types that use sound to injure, incapacitate, or kill a target.
New personal communications shows that infrasound can cause trough vibrations, resonance frequency about 7 Hz with internal organs of humans cause also cancer, such as colorectal cancer, colon cancer, pancreatic cancer, etc. (2, 3, 4) Some of these weapons have been described as sonic bullets, sonic grenades, sonic mines, or sonic cannons. Some USWs make a focused beam of sound or ultrasound, some made an area field of sound.
The LRAD Corporation says that anyone within a 100 meters of the device’s sound path will experience an extreme pain. The version generally utilized by Police Departments (the LRAD 500X) is designed to communicate at up to 2000 meters during ideal conditions. In a typical outdoor environment, the device can be heard for 650 meters. The 500X version is also capable of short bursts of directed sound that cause headaches in anyone within a 300 meter range. Anyone within 15 meters of the device’s audio path can experience permanent hearing loss. LRAD claims the device is not a weapon, but a directed-sound communication device…
Ultrasonic sound has very small wavelength in the millimeter range and lies beyond the threshold of human hearing.
This is an undeclared silent war
…























"Long Covid"? "Disease X"?
How much longer can this go on for?
Remarkable article, well done!